Tracheostomy and Ventilator Dependence
The scope of this page includes communication and swallowing issues in patients with tracheostomy, both with and without ventilator dependence, across the lifespan.
See the Tracheostomy and Ventilator Dependence Evidence Map for summaries of the available research on this topic.
Individuals with artificial airways due to medical complications often experience compromised communication and swallowing function. Speech-language pathologists (SLPs) with appropriate training contribute to the communication and swallow assessment and management of patients with tracheostomies, both with and without ventilator dependence, in cooperation with an interprofessional team.
Definitions relevant to page content:
- Artificial Airway: a device that is used to facilitate ventilation and secretion management (e.g., endotracheal tube, tracheostomy tube) and that may be used to access mechanical ventilation.
- Endotracheal tube (ET): a tube placed into the trachea via the mouth or nose to establish and/or maintain the airway and ventilation.
- Tracheotomy: a specific surgical procedure that involves an incision in the trachea and placement of a tube to create an artificial airway.
- Tracheostomy: the opening (tracheostoma) into the trachea created by the tracheotomy through which the tracheostomy tube can be inserted.
- Tracheostomy tube: a curved tube inserted into the tracheostoma to maintain an airway.
- Decannulation: the removal of a tracheostomy tube.
- Mechanical ventilator: a machine that assists or replaces the spontaneous breathing process.
Due to the wide variety of medical conditions that may necessitate a tracheostomy (both with and without mechanical ventilation), patients have diverse experiences in type and severity of communication and swallowing difficulties. Individualized assessment and management require interprofessional collaborative practice. A tracheostomy team may include an otolaryngologist, a pulmonologist, a respiratory therapist, nurses, and the SLP. Positive patient outcomes—including reductions in cannulation times, hospital length of stay, adverse events, and cost of care—have been realized when patients with tracheostomy are managed with a multidisciplinary team approach (Bonvento, Wallace, Lynch, Coe, & McGrath, 2017; de Mestral et al., 2011; Garrubba, Turner, & Grieveson, 2009). See ASHA's page on Interprofessional Education/Interprofessional Practice (IPE/IPP).
Other ASHA Practice Portal pages that are applicable to this topic include Adult Dysphagia, Pediatric Feeding and Swallowing, Voice Disorders, and Augmentative and Alternative Communication.
Incidence and Prevalence
A range of conditions (across the lifespan) may necessitate the placement and maintenance of an artificial airway, often leading to varying degrees of laryngeal injury and co-occurring communication and/or swallowing problems. A recent systematic review by Brodsky et al. (2018) found a high prevalence (83%) of laryngeal injury in adults who received endotracheal intubation with mechanical ventilation in the intensive care unit (ICU). Although the reasons for tracheostomy and severity of injuries varied across studies, dysphonia (76%), hoarseness (63%) and dysphagia (49%) were reported as common clinical symptoms post intubation. An additional systematic review by Skoretz, Flowers, and Martino (2010) reported the frequency of dysphagia in medical and surgical populations ranging from 3% to 62%, with higher frequencies noted with prolonged intubation (> 24 hours).
In the United States, it is also estimated that 800,000 people require mechanical ventilation each year (Mehta, Syeda, Wiener, & Walkey, 2015; Wunsch et al., 2010), with prolonged mechanical ventilation reported in approximately 250,000 (≥ 96 hours; Zilberberg, Luippold, Sulsky, & Shorr, 2008). As the aging population increases, these numbers are expected to rise with approximately 600,000 people requiring prolonged mechanical ventilation by the year 2020 (Stephan et al., 2013; Zilberberg, de Wit, & Shorr, 2012; Zilberberg & Shorr, 2008). Additional data revealed that 100,000 tracheostomies are performed each year on individuals requiring mechanical ventilation (Herritt, Chaudhuri, Thavorn, Kubelik, & Kyeremanteng, 2018; Shah et al., 2012).
Roles and Responsibilities
SLPs play a central role in the screening, assessment, diagnosis, and treatment of persons with swallowing and/or communication disorders related to artificial airways, including tracheostomies, with and without ventilator dependence. The professional roles and activities in speech-language pathology include clinical/educational services (diagnosis, assessment, planning, and treatment), advocacy, administration, and research. See ASHA's Scope of Practice in Speech-Language Pathology (ASHA, 2016).
Assessment and treatment of persons with swallowing and/or communication disorders related to artificial airways, including tracheostomies, with and without ventilator dependence may require use of appropriate personal protective equipment.
Appropriate roles for SLPs include, but are not limited to, the following:
- Maintaining general knowledge of the anatomy, physiology, and pathophysiology of the swallowing mechanism and the respiratory system
- Educating other professionals on the role of the SLP in the care of patients with tracheostomy, both with and without ventilator dependence
- Incorporating evidence-based practice into clinical care
- Collaborating with other professionals as a member of a tracheostomy team
- Identifying the signs and symptoms of dysphagia
- Identifying the signs and symptoms of communication disorders and delays
- Identifying the signs and symptoms of voice disturbance
- Conducting a culturally and linguistically appropriate comprehensive dysphagia assessment, including noninstrumental and instrumental assessments of swallow function in collaboration with other professionals, as appropriate
- Conducting a culturally and linguistically appropriate comprehensive communication assessment, including identification of potential communication vulnerability (Blackstone, Garrett, & Hasselkus, 2011)
- Assessing voicing options as well as nonverbal and augmentative and alternative communication options
- Documenting accurate and comprehensive information and data for each patient interaction
- Collaborating with other professionals (i.e., tracheostomy team) as well as the patient and significant others regarding the management of swallowing and communication disorders in patients with tracheostomy, both with and without ventilator dependence
- Providing safe and effective treatment for swallowing and communication disorders
- Determining candidacy for and appropriateness of using a speaking valve, capping trials, or a talking tracheostomy tube
- Facilitating safe and effective use of a speaking valve or specialty tracheostomy tube
- Providing education and counseling to patients, caregivers, and significant others, as appropriate
- Providing training and education regarding use of augmentative and alternative communication
- Referring to other professionals as appropriate to ensure comprehensive care and best outcomes
- Facilitating the inclusion of a child with a tracheostomy, with or without ventilator dependence, into school activities in collaboration with the medical team
- Using appropriate functional outcome measures
- Providing quality control and risk management
- Advocating for individuals requiring tracheostomy, both with and without ventilator dependence
- Contributing to performance improvement and research in communication and swallowing disorders
Essential Knowledge
Safe intervention for the patient with a tracheostomy tube, with or without ventilator dependence, requires essential knowledge of the following:
- The anatomy, physiology, and pathophysiology of the swallowing mechanism and the respiratory system
- A variety of medical conditions that may necessitate tracheostomy, both with and without mechanical ventilation, and their potential impacts on oral/verbal communication, swallowing, and quality of life
- Tracheostomy tube design—including various types, sizes, and components—and rationale for the use of each tube
- The physiologic changes in voice, swallowing, and respiration that occur secondary to tracheostomy, both with and without mechanical ventilation
- How to monitor physiological changes during assessment or therapy, and how to intervene as needed
As indicated in the Code of Ethics (ASHA, 2023), SLPs who serve this population should be specifically educated and appropriately trained to do so.
Populations Requiring Tracheostomy With or Without Mechanical Ventilation
SLPs may encounter patients with tracheostomy, both with and without ventilator dependence, in a variety of settings—including hospitals, skilled nursing facilities, rehabilitation centers, outpatient clinics, long-term acute care centers, schools, and home health care.
Patient populations requiring a tracheostomy (with or without the use of a mechanical ventilator) include those with diagnoses specific to lung disease, diagnoses impacting respiratory musculature, and/or diagnoses impacting structure and function of the respiratory tract, including the upper airway. Examples of patient diagnoses include the following:
- Cancer resection and reconstructive surgery (e.g., laryngeal/hypopharyngeal cancers)
- Cardiopulmonary diseases/conditions (e.g., congestive heart failure)
- Complications with premature birth and/or low birth weight (e.g., neonatal respiratory distress syndrome)
- Craniofacial or tracheoesophageal anomaly (e.g., micrognathia in Pierre Robin sequence)
- Neurological disorder/disease (e.g., stroke)
- Neuromuscular diseases/conditions (e.g., amyotrophic lateral sclerosis [ALS], muscular dystrophy)
- Prematurity/low birth weight
- Respiratory diseases/conditions (e.g., bronchopulmonary dysplasia, chronic obstructive pulmonary disease)
- Trauma (e.g., spinal cord injury, traumatic brain injury)
- Upper airway obstruction or edema (e.g., head and neck cancer, edema of the upper airway)
Tracheostomy
Among patient populations requiring a tracheostomy, the reasons for surgical intervention are varied, and the type of tracheostomy tube selected by the surgeon is individualized.
Indications for Tracheostomy
Surgical intervention and placement of a tracheostomy tube may address the following:
- Need for long-term mechanical ventilation
- Need for permanent tracheostomy tube (e.g., due to tracheal stenosis)
- Poor secretion management—tracheostomy tube allows for suctioning of secretions in the lower airway
- Prolonged intubation—which may result in laryngeal injury, patient discomfort, communication, and swallowing problems
- Upper airway obstruction
Tracheostomy Tubes
The type of tracheostomy tube placed by the surgeon will depend on the specific needs, characteristics, and medical status of the individual patient. Consideration is taken regarding the advantages offered and/or disadvantages imposed by each type of tube and its components.
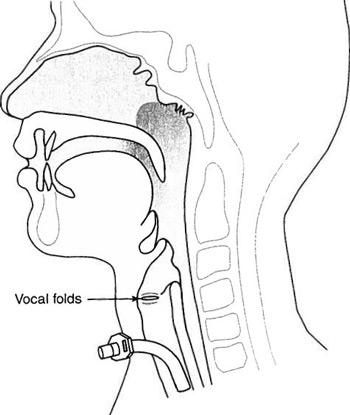
Figure 1: A tracheostomy tube in situ. From Communication and Swallowing Management of Tracheostomized and Ventilator-Dependent Adults (2nd ed) (p. 69) by K. J. Dikeman and M. S. Kazandjian, 2003, Clifton Park NY: Delmar Learning. Copyright 2003 by authors. Reprinted with permission.
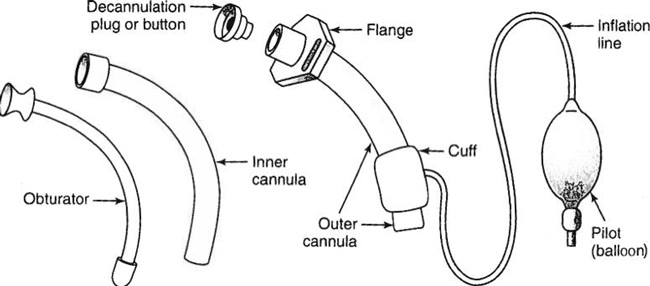
Figure 2. Parts of a standard tracheostomy tube. From Communication and Swallowing Management of Tracheostomized and Ventilator-Dependent Adults (2nd ed) (p. 86) by K. J. Dikeman and M. S. Kazandjian, 2003, Clifton Park NY: Delmar Learning. Copyright 2003 by authors. Reprinted with permission.
Types of Tracheostomy Tubes
Different types of tracheostomy tubes may include the following characteristics or specializations:
- Material variations: tubes can be made of metal (stainless steel), plastic (PVC), silicone, or polyurethane.
- Disposable versus reusable.
- Single lumen (outer cannula only) versus double lumen (outer and inner cannula); most pediatric tracheostomy tubes have only the outer cannula.
- Cuffed versus cuffless (i.e., presence or absence of tracheostomy tube cuff).
- Nonfenestrated (standard tube) versus fenestrated (has a hole in the cannula that allows air to pass from the trachea through the vocal folds).
- If the tracheostomy tube has an inner cannula, it must also be fenestrated (or removed) to take advantage of this option.
- Extended length tracheostomy tubes (XLT): can be distal XLT or proximal XLT.
- Talking tracheostomy: allows for voicing while tracheostomy tube cuff remains inflated (these patients are often ventilator dependent) with use of separate air sources for ventilation and phonation.
- Specialty cannula: allows for voicing while tracheostomy tube cuff remains inflated (e.g., speech cannula with flaps for directing exhaled air to the upper airway).
- Tracheostomal maintenance devices (e.g., tracheostomy button, long-term cannula): may replace the tracheostomy tube as a method of maintaining the open stoma (tracheal airway).
The type, size, and characteristics of a patient's tracheostomy tube may require alterations as a result of anatomical growth, changes in the patient's underlying condition, and/or facilitation of communication options.
Components of Tracheostomy Tubes
The components of a tracheostomy tube include the following:
- Outer cannula – the main body of the tracheostomy tube that fits directly into the tracheal stoma.
- Inner cannula – an inner tube that fits inside the outer cannula (in a dual cannula tube), which can be disposable or reusable and may be removed to assist in cleaning and prevention of mucus plugging.
- Cannulas are measured by inner/outer diameter and length of tube.
- Hub/connector – the external part of the tracheostomy tube cannula that allows for attachment to a mechanical ventilator or a speech valve.
- Neck flange – a neck plate that is labeled with dimensions and type of tracheostomy tube and is attached to tracheostomy ties to secure the tube in place.
- Obturator – an instrument used during the placement of the tracheostomy tube into the tracheostoma to guide insertion and prevent tissue damage; it is removed immediately after tube placement.
- Button/cap/plug – a component used to occlude the opening of the tracheostomy tube, which may be used during the weaning and decannulation process and may be quickly removed if necessary.
- Cuff – an inflatable “balloon” located on the distal part of the outer cannula, which can be inflated to prevent airflow into the upper airway.
- An inflated cuff is typically used during mechanical ventilation.
- Most cuffs are inflated with air; however, some can be made with foam.
- Pilot balloon – located at the distal end of an external inflation line, it indicates whether the cuff is inflated or deflated.
Tracheostomy Tube Considerations
Tube Size
An appropriately sized tracheostomy tube is important for addressing the communication and swallowing needs of patients with tracheostomy tubes. Tracheostomy tubes may be custom fit. When determining the appropriate size (i.e., inner diameter, outer diameter, length) of the tracheostomy tube, the tracheostomy team considers the following patient specifics:
- Age of patient (pediatric versus adult)
- Communication/speech needs
- Indications for tracheostomy procedure
- Lung mechanics
- Size of trachea
- Upper airway resistance/airway clearance
- Ventilation
(Mitchell et al., 2013; Sherman et al., 2000)
Cuff Status
Consideration of tracheostomy tube cuff status requires input from the tracheostomy team with attention to a patient's medical status, respiratory/ventilatory status, and the impact it has on the patient's communication status and swallow function. It is important to note that an inflated cuff does not prevent aspiration. If there is liquid at the level of the cuff, the patient has already aspirated as the cuff is located below the true vocal folds. Leakage around the cuff is possible; an inflated cuff does not provide a watertight seal.
Benefits of cuff deflation may include the following:
- Ability to place a one-way speaking valve (or otherwise occlude the stoma) to allow for
- voice production and
- generation of airflow for cough and throat-clear via the upper airway for improved airway clearance and protection.
- Reduced risk of damage to the tracheal wall caused by long-term cuff inflation.
- Potential improvements in swallow physiology (Amathieu et al., 2012; Davis, Bears, Barone, Corvo, & Tucker, 2002; Ding & Logemann, 2005; Hernandez et al., 2013).
Timing of Tube Change
The timing of the initial tracheostomy tube change may have an impact on patient progress. For example, changing the tube within a week of the tracheotomy procedure may result in earlier use of a speaking valve and earlier oral intake in adult patients (Fisher et al., 2013). Deutsch (1998) concluded that most pediatric tracheostomy tubes can be safely changed 3–4 days after surgery and that shorter intervals between surgery and the first tracheostomy tube change may be beneficial (e.g., shorter hospital stays).
Mechanical Ventilation
Mechanical ventilators are utilized with various modes and settings, which may require modifications as a patient's status or condition changes. Decisions made by the physician (e.g., pulmonologist) about the ventilator modes and/or settings are carried out by trained medical professionals.
Indications for Mechanical Ventilation
Mechanical ventilation is used to address compromised breathing, which impacts the ability to move air in and out of the lungs and/or for the lungs to complete the necessary gas exchange. Respiratory or ventilatory failure (or impending failure) is an indicator of the need for mechanical ventilation. Respiratory failure may be hypoxemic (i.e., abnormally low levels of oxygen in the blood) or hypercapnic (i.e., excess carbon dioxide in the blood). There are many and various etiologies of respiratory failure, including the following:
- Lung disease (e.g., chronic obstructive pulmonary disease [COPD], pneumonia)
- Multisystem failure or dysfunction (e.g., renal, cardiac)
- Impairment or injury of the anatomical or physiological respiratory mechanism (e.g., spinal cord injury, drug overdose, chest trauma)
Mechanical ventilation may also be used with patients who undergo anesthesia (e.g., during surgery).
Ventilator Modes/Settings
Ventilator settings (the characteristics of ventilation provided) and modes (representing the method—the how and when—of inspiratory support), as well as any modifications of the same, are determined and managed by the physician (or the respiratory therapist/nurse/trained professional under physician's orders).
Ventilator Settings
The primary mechanical ventilator settings include the following:
- Mode of ventilation
- Tidal volume (Vt) – size of each breath from the ventilator (measured in cc or ml)
- Respiratory rate (RR) – number of breath cycles delivered by the ventilator per minute
- Fractional inspired oxygen concentration (FiO2) – percentage of oxygen delivered with any breath
- Positive end expiratory pressure (PEEP) — the positive pressure (measured in cm of water) that is constantly applied to the airway (pressure that remains in lungs at the end of expiration)
- Alarms — warn of possible dangers related to the patient-ventilator system
Ventilator Modes
Ventilator modes can be either volume controlled (VC) or pressure controlled (PC), referring to which aspect(s) of the breath that are pre-set and controlled by the ventilator. Commonly used modes of mechanical ventilation include the following:
- Assist control (AC), also known as continuous mandatory ventilation (CMV): Ventilator provides mandatory pre-set breaths as well as pre-set breaths in response to the patient's initiation of additional breaths
- Synchronized intermittent mandatory ventilation (SIMV): Ventilator provides mandatory pre-set breaths but allows the patient to breathe spontaneously between these breaths
- Pressure support ventilation (PSV): Ventilator provides positive airway pressure with each patient-initiated breath and terminates positive airway pressure at the end of inspiration (i.e., augments spontaneous breathing)
- Continuous positive airway pressure (CPAP): Ventilator provides continuous positive pressure during the patient's spontaneous respiratory cycle and can be used while patient is still intubated (e.g., during weaning) or noninvasively (e.g., via mask)
Cuff Status With Mechanical Ventilation
A mechanical ventilator may be used when the tracheostomy tube cuff is inflated or deflated.
Possible benefits of inflated cuff with mechanical ventilation (Dikeman & Kazandjian, 2003):
- Easier to maintain tidal volume and oxygen saturation because air/oxygen are not escaping through the upper airway.
- Possible reduction in secretions passing into the lower airway around the tracheostomy tube; however, leakage around the cuff can still happen because the cuff does not provide a watertight seal.
- Of note, cuff inflation does not prevent aspiration because aspiration happens above the level of the cuff at the vocal folds.
Possible benefits of deflated cuff, both with and without mechanical ventilation (Dikeman & Kazandjian, 2003):
- Reduced risk of tissue trauma
- Normalized airflow through upper airway
- Reestablishment of the ability to cough
- Oral communication options
Impact of Tracheostomy and Ventilator Dependence on Swallow and Communication
Tracheostomy tube placement, both with and without mechanical ventilation, may impact the patient's swallow function and communication ability in various ways. Medically complex patients may have multifactorial causes of communication and swallow problems.
- Consequences of tracheostomy and ventilator dependence on communication and psychosocial well-being may include
- aphonia/dysphonia (e.g., airflow not passing through the vocal folds);
- emotional or psychological responses (e.g., frustration, withdrawal);
- inability to communicate wants/needs to staff and caregivers, which may impact patient safety;
- pain/discomfort associated with communication attempts; and
- reduced mobility (e.g., reduced play in children, resulting in limited opportunities for neurodevelopment).
- Consequences of tracheostomy and ventilator dependence on swallow function may include
- disrupted breathing pattern and coordination with swallow;
- increased risk of dysphagia and aspiration (Cameron, Reynolds, & Zuidema, 1973; Davis & Stanton, 2004; Elpern, Scott, Petro, & Ries, 1994; Leder, 2002; Tolep, Getch, & Criner, 1996);
- laryngeal/pharyngeal atrophy due to lack of airflow and disuse;
- need for alternative forms of nutrition and hydration to maintain proper nutritional status;
- reduced/absent cough response and subglottic pressure (e.g., for expectoration of secretions);
- reduced laryngeal sensitivity;
- reduced secretion management; and
- reduced smell and taste.
Issues in Swallowing With Tracheostomy
The assessment and treatment of dysphagia in patients with a tracheostomy (with or without ventilator support) does involve special considerations; however, the processes, procedures, approaches, and techniques used by the clinician are comparable. See the information on assessment and treatment in the ASHA Practice Portal pages on Adult Dysphagia and Pediatric Feeding and Swallowing as well as the summaries of available research in the Dysphagia (Adults) Evidence Map and the Pediatric Feeding and Swallowing Evidence Map for more detailed information.
Swallow Assessment
It is important to obtain answers to practical questions (as relevant to the age and developmental status of the patient) at the outset of a swallowing assessment and/or examination of feeding issues. Such questions may include the following:
- Is the patient medically stable?
- What is the patient's current level of alertness?
- What is patient's current mode of communication?
- What is the patient's current level of cooperation?
- What are the patient's positioning status and precautions?
- What is the nature of reflex and state behaviors in pediatric patients?
- Is the patient's condition temporary, permanent, degenerative, or developmental?
- What is the estimated timeframe for a tracheostomy tube (with or without ventilator support) to remain in place?
An association between dysphagia (e.g., aspiration/silent aspiration) and tracheostomy placement (both with and without ventilator dependence) has long been documented (Cameron et al., 1973; Davis & Stanton, 2004; Elpern et al., 1994; Leder, 2002; Tolep et al., 1996). A dysphagia screening may help determine the likelihood that dysphagia exists and inform decisions on further swallowing assessment. The goal of a dysphagia screening for patients with a tracheostomy/ventilator support is to identify key factors such as level of arousal and cooperation, oral motor skills, secretion management, and volitional swallow and cough ability that can help determine a patient's readiness for clinical and/or instrumental evaluations. It is not necessary for a patient to be weaned from the ventilator to begin the swallow assessment process.
A clinical swallow evaluation may be useful in identifying gross aspiration and overt signs and symptoms of feeding and swallowing difficulty and in determining a patient's readiness for follow-up instrumental measures, such as fiberoptic endoscopic evaluation of swallowing (FEES) and videofluoroscopic swallowing study (VFSS). Clinicians use instrumental swallow measures to fully assess the physiology/pathophysiology of the patient's swallow, including the presence or absence of (silent) aspiration, and to determine the appropriateness and effectiveness of a variety of treatment strategies. Reassessment may be warranted on an ongoing basis, as results will guide treatment. The ASHA Practice Portal pages on Adult Dysphagia and Pediatric Feeding and Swallowing provide in-depth information on both instrumental and clinical (noninstrumental) dysphagia assessments. See the Tracheostomy and Ventilator Dependence Evidence Map for summaries of the available research on swallow assessment in this population.
When working with the population of patients with tracheostomy (both with and without ventilator dependence), the clinician addresses the following questions before, during, and after the assessment process (as appropriate to the age and developmental status of the patient):
- What is the patient's current medical status?
- Presence of comorbidities
- Vital signs
- Oral hygiene status and practices
- What is the patient's current respiratory status (including contraindications to oral intake)?
- Level of ventilator support (if any)
- Supplemental oxygen requirements
- Frequency and type of suctioning
- Secretions (e.g., oral/tracheal, amount, type, consistency) and secretion management
- What is the patient's current nutritional status?
- Current mode of intake
- Current restrictions
- Any alternate nutrition in place (e.g., nasogastric tube or gastrostomy tube)
- Length of time without oral intake (if at all)
- Patient interest in oral intake
- Was the patient intubated before tracheostomy? If yes, for how long and how many times?
- When and why was the tracheotomy performed? (trauma, bleeding, and edema can be present initially from procedure)
- What is the size and type of the tracheostomy tube (e.g., fenestrated, extended-length)?
- If cuffed, what is the status—deflated, partly inflated, or fully inflated?
- Does the patient tolerate at least partial cuff deflation?
- Cuff deflation/reduced cuff pressure may positively impact swallow function (Amathieu et al., 2012; Davis et al., 2002; Ding & Logemann, 2005).
- Does the patient (off mechanical ventilation) tolerate tracheal occlusion?
- Is the patient using (or, are they a candidate to begin using) a speaking valve?
- Speaking valve use may positively impact swallow function in some patients (Dettelback, Gross, Mahlmann, & Eibling, 1995; Elpern, Okonek, Bacon, Gerstung, & Skrzynski, 2000; Suiter, McCullough, & Powell, 2003).
- Is the patient able to phonate, and with what vocal quality?
- Is the patient able to clear their throat and/or cough for airway protection and clearance (spontaneous or elicited)?
- What is the patient's pain level with swallow?
- Will the patient be on or off the ventilator when eating (e.g., during weaning trial)?
Swallow Treatment
Special considerations in the treatment of dysphagia in patients with a tracheostomy (with or without ventilator dependence) include the following (dependent upon the patient's age and developmental status):
- Emphasize and assist in proper oral and tracheostomy hygiene protocols as developmentally appropriate
- Provide oral stimulation and nonnutritive sucking procedures (when working with the infant population)
- Consult with the patient-care team to determine the best physical positioning for the patient during swallow treatment
- Monitor the patient's health status/vitals and provide or obtain suction as needed (e.g., with clearance or assist from physician, nurse, or respiratory therapist) during any treatment activities
- Monitor the patient's respiratory/pulmonary status as well as ventilation needs (if patient is on a ventilator), and collaborate with care team (e.g., physician, respiratory therapist, nurse) for management/adjustments as appropriate and necessary
- For patients who tolerate cuff deflation and speaking valve placement, deflate cuff and place a speaking valve during treatment to normalize airflow and air pressures, restore sensory function in the upper airway, improve postural stability, and possibly reduce aspiration risk
- Use traditional swallow therapy and/or diet modifications, as appropriate
- Initiate early rehabilitative exercise, as indicated
- Consider risks associated with traditional compensatory strategies or postures when used by a patient with a tracheostomy (e.g., the chin-tuck posture may create a risk of dislodging the tracheostomy tube)
- Use direct (with use of food or liquid) and indirect (without use of food or liquid) treatment, as appropriate
- Consult with physical therapists, respiratory therapists, and other specialists, as indicated (e.g., pulmonary rehabilitation, respiratory muscle strength training [RMST])
Suctioning With Tracheostomy Tube In Situ
ASHA's Code of Ethics stipulates that clinicians must be competent in any area in which they practice. ASHA's Scope of Practice in Speech-Language Pathology is broad and does not address specific procedures; however, procedures should be related to the assessment and treatment of patients with communication or swallowing disorders. Some facilities (e.g., hospitals) have a process in place for “credentialing” staff in suctioning procedures and may provide training to SLPs in these procedures. It is important to consider potential liability associated with tracheostomy-related procedures, such as changing or capping tracheotomy tubes.
State licensure laws vary. Some states may provide specific guidance, whereas others do not. It is the clinician's responsibility to be aware of laws and guidelines applicable to each situation. See also ASHA's Position Statement on Multiskilled Personnel and Technical Report on Multiskilled Personnel.
Issues in Communication With Tracheostomy
There are specific considerations when assessing and treating communication in individuals with tracheostomy (with or without ventilator dependence). Depending on the patient's diagnoses, age, needs, strengths/weaknesses, and goals, the information on assessment and treatment in the following ASHA Practice Portal pages may be helpful: Acquired Apraxia of Speech, Aphasia, Augmentative and Alternative Communication, Pediatric Traumatic Brain Injury, and Traumatic Brain Injury in Adults.
Communication Assessment
The approach to providing a communication assessment to a patient with a tracheostomy, with or without ventilator dependence, involves special considerations. These considerations may be addressed by answering/considering the following questions (as appropriate to the patient's age and developmental status):
- Is the patient's medical condition temporary, permanent, progressive/degenerative, or developmental (e.g., present at or shortly after birth)?
- How long will the artificial airway likely be in place, and how will this affect short- and long-term communication?
- If ventilated, are there any adjustments that can be made to improve speech communication (Hoit, Banzett, Lohmeier, Hixon, & Brown, 2003; Prigent et al., 2010)?
- How do the following factors affect the choice of the most appropriate communication method?
- Level of alertness/attentiveness/responsiveness
- Voicing abilities (e.g., no audible phonation, reduced quality or intensity)
- Respiratory status (including respiratory endurance and breath coordination)
- Vocal hygiene status
- Verbal fluency and ease/difficulty of speech production
- Cognitive abilities
- Language abilities
- Developmental abilities
- Motor status
- Behaviors and emotions surrounding the artificial airway (e.g., anxiety, depression, agitation)
- Cooperation and motivation
- Does the patient have comorbid speech and language disorders (e.g., aphasia)?
- Will they need a mixture of communication options (e.g., high-tech and low-tech, oral and nonoral)?
- Which option(s) best meet the needs and goals of the patient and the family/caregivers?
Communication Treatment
The approach to providing communication treatment to patients with tracheostomy, with or without ventilator dependence, involves special considerations.
Communication choices for people with artificial airways may include both high-tech and low-tech augmentative and alternative communication (AAC) options as well as both oral and nonoral options. Several options may be appropriate for a patient, depending upon their situation. Options include the following (as appropriate for the patient's age and developmental status):
- Nonverbal and nonoral communication options may include
- writing;
- texting;
- signing (varied forms or sign language);
- tablet or phone apps;
- low-tech AAC; and
- high-tech AAC.
- Verbal communication options may include
- mouthing of words with lip reading by the communication partner;
- use of leak speech with partial or full cuff deflation (using air leaking around the tracheostomy tube and passing over the vocal folds);
- use of an electrolarynx;
- use of digital occlusion, capping, or plugging the tracheostoma (with a noncuffed or cuff-deflated tracheostomy tube);
- use of a talking tracheostomy tube;
- use of a speaking valve; and
- use of ventilator adjustments for speech (Hoit et al., 2003; Prigent et al., 2010).
Verbal communication options may require modification to the current tracheostomy tube (or a change in type of tube), cuff inflation status, and/or ventilator settings. These changes will involve input from the tracheostomy team members (e.g., SLP, nurse, respiratory therapist, physician). It is always prudent for a patient with a tracheostomy tube to have a nonoral backup system of communication.
One-Way Speaking Valves
One-way speaking valves enable individuals with a tracheostomy tube to use voice and speech to communicate. A variety of speaking valves are available. Although each available speaking valve may look and work somewhat differently, in general, they close on expiration and redirect expired air through the upper airway and vocal folds. Some speaking valves can be placed in line with a ventilator. Early speech intervention and voice restoration for a patient with mechanical ventilation may lead to increased participation in their care and improved quality of life (Freeman-Sanderson, Togher, Elkins, & Phipps, 2016). Candidacy for speaking valve use must be carefully established.
Candidacy requirements for safe and effective speaking valve placement and use include the following (Hess & Altobelli, 2014):
- Must be medically stable (e.g., no current infection)
- Must tolerate cuff deflation (if using a cuffed tracheostomy tube)
- Must be able to exhale around the tracheostomy tube and through the upper airway
- Must maintain adequate/acceptable oxygen saturation, respiratory rate, and heart rate when the valve is in place
Candidacy considerations may also include the following (Hess & Altobelli, 2014):
- May require a tracheostomy tube downsize or change in type of tracheostomy tube
- May require changes in vent settings
- May need to overcome anxiety or discomfort associated with speaking valve placement and redirection of airflow
- In infants and young children, overt negative behaviors with speaking valve placement may be physiological and/or behavioral.
Benefits of speaking valve use may include the following:
- Improved vocal quality, intensity, fluidity, and length of utterances during connected speech
- Improved cough and secretion management
- Increased upper airway sensation including olfaction
- Possible benefits to swallowing function (which can be identified during the swallow assessment)
- Improved quality of life and self-advocacy
Contraindications for speaking valve use include the following:
- Unconscious patients
- Foam cuff tracheostomy tube
- Inflated tracheostomy tube cuff
- Significant airway obstruction, which may prevent sufficient exhalation
- Laryngectomy
- Unmanageable copious and/or thick secretions
- High ventilator settings (e.g., rate, PEEP settings)
- Medical instability
Considerations For Pediatric Populations
When working with pediatric populations, including infants and neonates, SLPs must be aware of the following special considerations:
- Recognizing anatomical and pathophysiologic differences between adults and infants/children
- Being familiar with the characteristics of pediatric tracheostomy tubes, which may differ from those used with adults
- Attending to responses to pain and discomfort (which may not be communicated verbally), such as cries, facial expressions, unusual postures, and agitated movements
- Understanding the timing of tracheostomy tube placement as it relates to the critical time period for speech, language, and sensorimotor development
- Modifying the environment, patient positioning, and patient handling to achieve and maintain the child's ability to move around and to support normal development of gross motor skills (i.e., ensure physical therapy or occupational therapy consult[s], as indicated)
- Addressing feeding concerns and nonnutritive oral stimulation, as indicated
- Providing ongoing assessment with attention to parent/caregiver experience, including caregiver stress, comfort during interaction, and ability to facilitate positive cognitive communication development
- Using assessment measures specific to the pediatric population (i.e., age range and developmental status)
- Embracing and collaborating with a multidisciplinary care team (e.g., SLP, physicians, nurses, physical therapists, occupational therapists, respiratory therapists, psychologists, school personnel)
- Using treatment tools and strategies appropriate for the pediatric population (i.e., age and developmental status)
- Assisting with the necessary training to increase the parent/caregiver's comfort with tracheostomy and/or ventilator care
- Establishing a plan of care specific to the patient's and the family/caregiver's priorities and goals
- Establishing a plan of care accounting for the consequences of short- and long-term tracheostomy in the pediatric population
As with all populations (and especially relevant to pediatric populations), providing holistic, interprofessional, and patient/family-centered care is crucial in achieving the best outcomes.
ASHA Resources
- Aerosol Generating Procedures
- End-of-Life Issues in Speech-Language Pathology
- International Classification of Functioning, Disability, and Health (ICF)
- Interprofessional Education/Interprofessional Practice (IPE/IPP)
- Position Statement: Multiskilled Personnel
- Special Interest Group 13, Swallowing and Swallowing Disorders (Dysphagia)
- Technical Report: Multiskilled Personnel
Other Resources
This list of resources is not exhaustive and the inclusion of any specific resource does not imply endorsement from ASHA.
- American Academy of Otolaryngology-Head and Neck Surgery
- American Thoracic Society
- International Ventilator Users Network
- Passy-Muir
- The Global Tracheostomy Collaborative
- The New Zealand Speech-language Therapists' Association - Position Statement: Tracheostomy Management [PDF]
- United Kingdom National Tracheostomy Safety Project
Amathieu, R., Sauvat, S., Reynaud, P., Slavov, V., Luis, D., Dinca, A., . . . Dhonneur, G. (2012). Influence of the cuff pressure on the swallowing reflex in tracheostomized intensive care unit patients. British Journal of Anaesthesia, 109, 578–583.
American Speech-Language-Hearing Association. (2016). Scope of practice in speech-language pathology [Scope of Practice]. Available from www.asha.org/policy/.
American Speech-Language-Hearing Association. (2023). Code of Ethics [Ethics]. Available from www.asha.org/policy/.
Blackstone, S., Garrett, K., & Hasselkus, A. (2011). New hospital standards will improve communication: Accreditation guidelines address language, culture, vulnerability, health literacy. The ASHA Leader, 16, 24–25. Retrieved from https://leader.pubs.asha.org/doi/10.1044/leader.OTP.16012011.24
Bonvento, B., Wallace, S., Lynch, J., Coe, B., & McGrath, B. A. (2017). Role of the multidisciplinary team in the care of the tracheostomy patient. Journal of Multidisciplinary Healthcare, 10, 391–398.
Brodsky, M. B., Levy, M. J., Jedlanek, E., Pandian, V., Blackford, B., Price, C., . . . Akst, L. M. (2018). Laryngeal injury and upper airway symptoms after oral endotracheal intubation with mechanical ventilation during critical care: A systematic review. Critical Care Medicine, 46, 2010–2017.
Cameron, J. L., Reynolds, J., & Zuidema, G. D. (1973). Aspiration in patients with tracheostomies. Surgery, Gynecology & Obstetrics, 136, 68–70.
Davis, D. G., Bears, S., Barone, J. E., Corvo, P. R., & Tucker, J. B. (2002). Swallowing with a tracheostomy tube in place: Does cuff inflation matter? Journal of Intensive Care Medicine, 17, 132–135.
Davis, L. A., & Stanton, S. T. (2004). Characteristics of dysphagia in elderly patients requiring mechanical ventilation. Dysphagia, 19, 7–14.
de Mestral, C., Iqbal, S., Fong, N., LeBlanc, J., Fata, P., Razek, T., & Khwaja, K. (2011). Impact of a specialized multidisciplinary tracheostomy team on tracheostomy care in critically ill patients. Canadian Journal of Surgery, 54, 167–172.
Dettelbach, M. A., Gross, R. D., Mahlmann, J., & Eibling, D. E. (1995). Effect of the Passy‐Muir valve on aspiration in patients with tracheostomy. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck, 17, 297–302.
Deutsch, E. S. (1998). Early tracheostomy tube change in children. Archives of Otolaryngology–Head & Neck Surgery, 124, 1237–1238.
Ding, R., & Logemann, J. A. (2005). Swallow physiology in patients with trach cuff inflated or deflated: A retrospective study. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck, 27, 809–813.
Dikeman, K. J., & and Kazandjian, M. S. (2003). Communication and swallowing management of tracheostomized and ventilator-dependent adults (2nd ed.). Clifton Park, NY: Delmar Learning.
Elpern, E. H., Okonek, M. B., Bacon, M., Gerstung, C., & Skrzynski, M. (2000). Effect of the Passy-Muir tracheostomy speaking valve on pulmonary aspiration in adults. Heart & Lung, 29, 287–293.
Elpern, E. H., Scott, M. G., Petro, L., & Ries, M. H. (1994). Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest, 105, 563–566.
Fisher, D. F., Kondili, D., Williams, J., Hess, D. R., Bittner, E. A., & Schmidt, U. H. (2013). Tracheostomy tube change before day 7 is associated with earlier use of speaking valve and earlier oral intake. Respiratory Care, 58,257–263.
Freeman-Sanderson, A., Togher, L., Elkins, M., & Phipps, P. (2016). An intervention to allow early speech in ventilated tracheostomy patients in an Australian intensive care unit (ICU): A randomised controlled trial. Australian Critical Care, 29, 114.
Garrubba, M., Turner, T., & Grieveson, C. (2009). Multidisciplinary care for tracheostomy patients: A systematic review. Critical Care, 13, R177.
Hernandez, G., Pedrosa, A., Ortiz, R., Accuaroni, M. D. M. C., Cuena, R., Collado, C. V., . . . Fernandez, R. (2013). The effects of increasing effective airway diameter on weaning from mechanical ventilation in tracheostomized patients: A randomized controlled trial. Intensive Care Medicine, 39, 1063–1070.
Herritt, B., Chaudhuri, D., Thavorn, K., Kubelik, D., & Kyeremanteng, K. (2018). Early vs. late tracheostomy in intensive care settings: Impact on ICU and hospital costs. Journal of Critical Care, 44, 285–288.
Hess, D. R., & Altobelli, N. P. (2014). Tracheostomy tubes. Respiratory Care, 59, 956–973.
Hoit, J. D., Banzett, R. B., Lohmeier, H. L., Hixon, T. J., & Brown, R. (2003). Clinical ventilator adjustments that improve speech. Chest, 124, 1512–1521.
Leder, S. B. (2002). Incidence and type of aspiration in acute care patients requiring mechanical ventilation via a new tracheotomy. Chest, 122, 1721–1726.
Mehta, A. B., Syeda, S. N., Wiener, R. S., & Walkey, A. J. (2015). Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. Journal of Critical Care, 30, 1217–1221.
Mitchell, R. B., Hussey, H. M., Setzen, G., Jacobs, I. N., Nussenbaum, B., Dawson, C., . . . Merati, A. (2013). Clinical consensus statement: Tracheostomy care. Otolaryngology–Head and Neck Surgery, 148, 6–20.
Prigent, H., Garguilo, M., Pascal, S., Pouplin, S., Bouteille, J., Lejaille, M., . . . Lofaso, F. (2010). Speech effects of a speaking valve versus external PEEP in tracheostomized ventilator-dependent neuromuscular patients. Intensive Care Medicine, 36, 1681–1687.
Shah, R. K., Lander, L., Berry, J. G., Nussenbaum, B., Merati, A., & Roberson, D. W. (2012). Tracheotomy outcomes and complications: A national perspective. TheLaryngoscope, 122, 25 –29.
Sherman, J. M., Davis, S., Albamonte-Petrick, S., Chatburn, R. L., Fitton, C., Green, C., . . . Zinman, R. (2000). Care of the child with a chronic tracheostomy. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. American Journal of Respiratory and Critical Care Medicine, 161, 297–308.
Skoretz, S. A., Flowers, H. L., & Martino, R. (2010). The incidence of dysphagia following endotracheal intubation: A systematic review. Chest, 137, 665–673.
Stephan, M. S., Shieh, M. S., Perkow, P. S., Rothberg, M. B., Steingrub, J. S., Lagu, T., & Lindenauer, P. K. (2013). Epidemiology and outcomes of acute respiratory failure in the United States, 2001–2009: A national survey. Journal of Hospital Medicine, 8, 76–82.
Suiter, D. M., McCullough, G. H., & Powell, P. W. (2003). Effects of cuff deflation and one-way tracheostomy speaking valve placement on swallow physiology. Dysphagia, 18, 284–292.
Tolep, K., Getch, C. L., & Criner, G. J. (1996). Swallowing dysfunction in patients receiving prolonged mechanical ventilation. Chest, 109, 167–172.
Wunsch, H., Linde-Zwirble, W. T., Angus, D. C., Hartman, M. E., Milbrandt, E. B., & Kahn, J. M. (2010). The epidemiology of mechanical ventilation use in the United States. Critical Care Medicine, 38, 1947–1953.
Zilberberg, M. D., de Wit, M., & Shorr, A. F. (2012). Accuracy of previous estimates for adult prolonged acute mechanical ventilation volume in 2020: Update using 2000–2008 data. Critical Care Medicine, 40, 18–20.
Zilberberg, M. D., Luippold, R. S., Sulsky, S., & Shorr, A. F. (2008). Prolonged acute mechanical ventilation, hospital resource utilization, and mortality in the United States. Critical Care Medicine, 36, 724–730.
Zilberberg, M. D., & Shorr, A. F. (2008). Prolonged acute mechanical ventilation and hospital bed utilization in 2020 in the United States: Implications for budgets, plant and personnel planning. BMC Health Services Research, 8, 242.
Acknowledgements
Content for ASHA's Practice Portal is developed through a comprehensive process that includes multiple rounds of subject matter expert input and review. ASHA extends its gratitude to the following subject matter experts who were involved in the development of the Tracheostomy and Ventilator Dependence page:
- Suzanne Abraham, PhD, CCC-SLP
- Carmin Bartow, MS, CCC-SLP
- Karen Dikeman, MA, CCC-SLP
- Alice Inman, MS, CCC-SLP
- Julie Kobak, MA, CCC-SLP
- Katy Peck, MA, CCC-SLP
- Donna Scarborough, PhD, CCC-SLP
- Stacey Skoretz, PhD, CCC-SLP
- Donna Tippett, MA, CCC-SLP
- Kathleen Wengel, MS, CCC-SLP
Citing Practice Portal Pages
The recommended citation for this Practice Portal page is:
American Speech-Language-Hearing Association (n.d.) Tracheostomy and Ventilator Dependence. (Practice Portal). Retrieved month, day, year, from www.asha.org/Practice-Portal/Professional-Issues/Tracheostomy-and-Ventilator-Dependence/.
Content Disclaimer: The Practice Portal, ASHA policy documents, and guidelines contain information for use in all settings; however, members must consider all applicable local, state and federal requirements when applying the information in their specific work setting.











